Abstract
Introduction: Mutations in TP53 are the most common mutations in human cancer and occur in almost every cancer subtype. In adult acute myeloid leukemia (AML), TP53 mutations, especially those associated with complex cytogenetics, are associated with a poor prognosis. However, given the rarity of TP53 mutations in pediatric AML, less is known about its prognostic significance.
Methods:TP53 variant status was determined in patients with AML enrolled on 4 successive COG trials for de novo pediatric AML (NCT00002798, NCT00070174, NCT01407757, NCT01371981). Next generation sequencing was retrospectively employed on diagnostic specimens to screen for variants including single nucleotide variants (SNVs) and insertions and deletions (indels). Variants were classified as benign, likely benign, unknown significance, likely pathogenic, and pathogenic using ClinVar and ACMG/AMP guidelines.
Results: Of 1790 patients (age: median 10.48 years, range 0.01-29.84 years), 68 (3.8%) had TP53 variants. Sixty-four (94.1%) of these were SNVs, 2 (2.9%) were in-frame indels, and 2 (2.9%) were frameshifts leading to early protein truncation. Twenty-six (38.2%) were considered likely pathogenic or pathogenic (TP53mut) (age: median 8.38 years, range 0.31-17.97 years), 33 (48.5%) considered likely benign or benign, and the remaining 9 (13.2%) were of unknown significance. Thirty-four (53.1%) TP53 SNVs fell within the DNA binding domain, including 100% of TP53mut SNVs (including many occurring at DNA binding sites).
We compared disease characteristics and clinical outcomes between patients with TP53mut and patients without any TP53 variant (TP53wt). Patients with non-pathogenic variants were excluded from the analysis. There was a higher prevalence of complex cytogenetics (defined as 3 or more chromosomal aberrations, including at least one structural aberration on karyotype) in TP53mut patients compared to TP53wt patients (55% vs. 18%; p=<.0001). There was no difference in the prevalence of co-occurring contemporarily defined high-risk alterations (TP53mut 30.8% vs. TP53wt 32.1%; p=0.879) but TP53mut patients were less likely to have co-occurring low-risk alterations compared to TP53wt patients (15.4% vs. 41.1%; p=0.008).
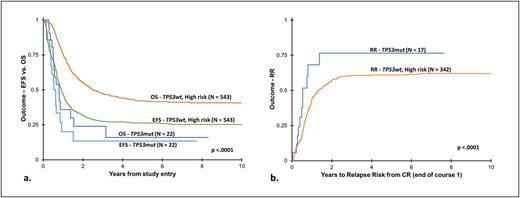
While there were no differences in complete remission rates (TP53mut 85% vs. TP53wt 77.6%; p=0.426) or their ability to clear minimal residual disease (TP53mut 55% vs. TP53wt 71.6%; p=0.132), TP53mut patients had a lower event-free survival (EFS) compared to TP53wt patients (5yr: 13.3% vs. 46.3%; p <.0001), which was largely driven by a higher relapse risk (RR) (5yr: 76.5% vs. 42.1%; p <.0001). Salvageability following an event was largely unsuccessful for TP53mut patients, including only 1 long-term survivor following an event, which contributed to a lower overall survival (OS) compared to TP53wt patients (5yr: 15.9% vs. 64.7%; p < .0001). Further, EFS (13.3% vs. 26.3%; p <.0001; Figure 1a), RR (5yr: 76.5% vs. 60.9%; p <.0001; Figure 1b) and OS (5yr: 15.9% vs. 42.1%; p <.0001; Figure 1a) were significantly inferior compared to contemporarily defined high-risk patients. When patients with co-occurring high-risk alterations were excluded from analysis, TP53mut patients maintained their poor 5-yr EFS (13.3%), RR (76.5%) and OS (15.9%).
Conclusions: In the largest study of TP53 mutations in pediatric patients with de novo AML, we show that pathogenic TP53variants are rare but prognostically significant. TP53mut patients were more likely to have complex cytogenetics and less likely to have co-occurring low-risk alterations. Outcomes for TP53mut patients were significantly inferior compared to contemporarily defined high-risk patients. Finally, these poor outcomes were maintained even when TP53mut patients with co-occurring high-risk lesions were excluded from analysis. Taken together, these data would suggest TP53 pathogenic mutations should be considered high-risk defining lesions in pediatric AML. Since HSCT is the standard of care for relapsed disease, the lack of salvageability following an event may suggest this disease is less alloreactive than other subtypes of AML, but further investigation is needed. Given the dismal outcomes after an event, clinical trials and novel targeted agents should be prioritized for relapsed patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal